Correct answer: e
Discussion
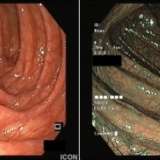
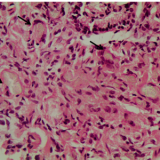
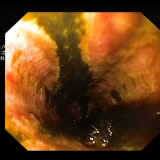
Nicorandil, a combined venous and arterial vasodilator, is now effectively the drug of last resort for angina. The reason is that numerous reports of ulceration affecting the skin, eyes or mucous membranes have accumulated since the drug was launched in 1994. Small apthous ulcers are said to occur in up to 5% of patients,1 but more severe, painful and deep ulceration may ensue. In the gastrointestinal tract, perforations, fistula formation and abscesses are recognised complications. Patients taking NSAIDs or steroids or who have diverticular disease are at particular risk. There is also some evidence that the risk of ulceration increases with dose and that ulceration may be precipitated by an increase in dose. The underlying mechanism by which the drug causes ulceration is unknown.
Nicorandil-induced ulcers persist until the drug is withdrawn, although healing may take up to 6 months. In this particular case, the ulceration would probably return after surgery if nicorandil was not identified as the underlying cause. In addition to ulceration, nicorandil is contraindicated in patients with hypokalaemia, heart failure and renal impairment.





Please log in with your myUEG account to post comments.