Correct answer: D.
Discussion
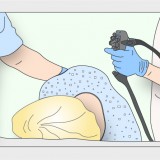
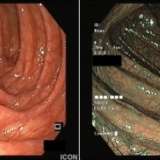
Acute oesophageal necrosis (AEN), more frequently known as black oesophagus, was first described in 1990.1It has been also described as Gurvits syndrome, after the physician whodescribed itin depthand studied it thoroughly.2As seen in the case patient, AEN is characterized by the conspicuous endoscopic finding of diffuse and circumferential black ulcero-necrotic oesophageal mucosa, almost always involving the distal oesophagus and with an abrupt demarcation line at the gastro-oesophageal junction.3
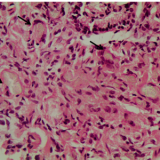
Biopsy samples are not required for confirmation of diagnosis unless there is a high degree of suspicion for the presence of atypical forms of infection (e.g. CMV or HSV oesophagitis). When biopsy samples are taken tissue necrosis of variable depth is noted, with accompanying ulcerations and deposits of hemosiderin.4
AEN is a rare entity, with an incidence of only 0.1–0.28%, being encountered most frequently in the older population (mean age 67 years) and with a predilection for the male sex.5Around 220 cases have been presented so far worldwide.2The vast majority of patients (>90%) present with signs of upper gastrointestinal bleeding. Other less frequent symptoms include nausea, fever, dysphagia and abdominal pain.6–8


Please log in with your myUEG account to post comments.