C. There is an adenoma with low-grade dysplasia
Decide on the Spot
An elusive lesion in the colon
November 05, 2019 | George Axiaris and Spyros Michopoulos
A 55-year-old female patient with no family history of colorectal cancer (CRC) underwent a scheduled screening colonoscopy.
The colonoscopy was performed by an experienced endoscopist (adenoma detection rate [ADR] of 54%), using a high-resolution colonoscope with narrow-band imaging (NBI) cabaility. Carbon dioxide was used for bowel insufflation.
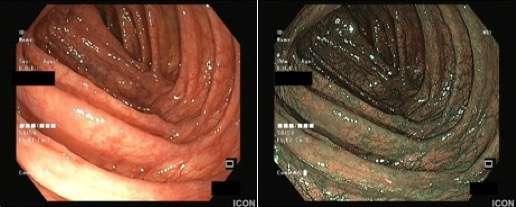
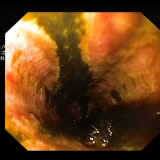
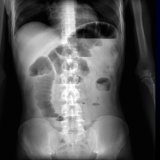
The patient was sedated with midazolam and propofol, with adequate oxygen supplementation and continuous monitoring of her blood pressure and oxygen saturation. The video shows the colonoscopy and two photos (figure 1) are provided of the ascending colon and of the area near the hepatic flexure during withdrawal of the scope.
Case question 1
Which of the following statements is correct?
A. There is a serrated lesion without dysplasia
B. There is a serrated lesion with dysplasia
C. There is an adenoma with low-grade dysplasia
D. There is an adenoma with high-grade dysplasia
-
Show case question answers 1
Case question 2
What is the minimum length of time you should spend inspecting the right colon (including the cecum, ascending colon and hepatic flexure)?
A. 3 minutes
B. 4 minutes
C. 5 minutes
D. 6 minutes
-
Show case question answers 2
D. 6 minutes
Case question 3
Which of the following is more likely to increase the adenoma detection rate (ADR)?
A. Better training
B. Chromoendoscopy
C. A mucosal exposure device/cap
D. All of the above
-
Show case question answers 3
D. All of the above (better training, chromoendoscopy, a mucosal exposure device/cap)
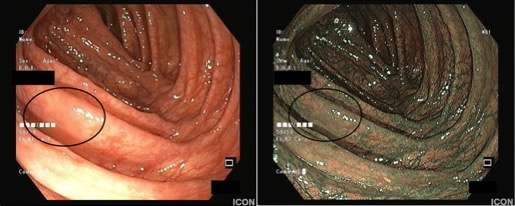
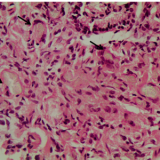
On careful inspection, a lesion is visible in the upper part of the patient’s ascending colon (figure 2). The polyp is 1.5cm in size, type IIa according to the Paris classification and NICE II after inspection with NBI. The lesion was subsequently resected via endoscopic mucosal resection (EMR) after submucosal injection of dilute adrenaline and indigo carmine. Histology revealed the lesion to be a tubulous adenoma with low-grade dysplasia.
[Caption für normales Artikel Motiv Bild ermöglichen! Single Image Galerie nicht sinnvoll.]
The measurement that best reflects how carefully colonoscopy is performed, especially screening colonoscopy, is the ADR. This rate is defined as the percentage of patients over the age of 50 undergoing screening colonoscopy in whom one or more precancerous polyps are detected. The ADR should be at least 30% in men and 20% in women (according to the ASGE Guidelines). 1
Withdrawal time — the time it takes to remove the scope from the colon — is also an important quality metric for colonoscopy. Several studies have shown that the ADR increases as the colonoscopy withdrawal time increases. The colonoscopy withdrawal time is considered more important than other parameters that impact the ADR (i.e. male sex, age >50 years, a personal or family history of CRC or colorectal polyps, a positive faecal occult blood test, and being the patient’s first [versus subsequent] colonoscopy) 2 because it is a modifiable factor related to the ADR. 3,4 The recommended minimum withdrawal time for screening colonoscopy is 6 minutes for the entire colon. 5 There are studies demonstrating that ADR is maximized with a total withdrawal time of 8–9 minutes or even 11 minutes, but with no additional benefit beyond 11 minutes. 6,7
But how much time should we spend in the area of the right colon? Appropriate withdrawal times for individual colonic segments are not well known. A recent study showed that adequate inspection of the right colon required at least 2 minutes. 8 The same study concluded that the ADR appeared to be significantly increased when withdrawal time was at least 2–4 minutes in the proximal colon and at least 3 minutes in the left colon, when compared with shorter withdrawal times. It should be noted that implementation of systematic monitoring and analysis of withdrawal time and ADR for each endoscopist may help to increase the ADR and improve the quality of colonoscopy offered. 9,10
Colonoscopy is a highly operator-dependent procedure and wide variations in ADRs have been reported for endoscopists. Several methods and devices have been implemented in order to improve the ADR of every endoscopist. 11
First of all, the fundamental role of training should not be overlooked. Appropriate training should be offered to all gastroenterologists in order that they comprehend the colonoscopy technique. Education should provide skills such as optical manoeuvring of the colonoscope, proper repositioning of the patient, adequate insufflation and lesion recognition and characterization.10 In addition, every gastroenterologist should seek further educational opportunities to remain up to date. Indeed, endoscopist training programs that apply simple educational methods have been shown to improve ADRs. 12
Changing the patient’s position is a useful tool, not only during scope insertion but also during withdrawal and can improve adenoma detection.13 The optimal positions for inspection are the left lateral decubitus position in the right colon, the supine position in the transverse colon and the right lateral decubitus position in the left colon. 11
Although the broad application of screening colonoscopy has reduced CRC mortality, mortality due to right colon cancer has not been equally improved. Double right colon examination is frequently performed and increases the ADR when compared with a single-pass examination. 14
Retroflexion is another nondevice-assisted method aimed at improving the ADR. Several studies have examined the value of retroflexion in the right colon, most of them with positive outcomes. 15 In a prospective study with high-resolution colonoscopes, the ADR was increased by using retroflexion in the ascending colon. 16 At times endoscopists are frustrated by colon motility that prevents proper mucosal visualization. Hyoscine N-butylbromide, an anticholinergic agent, has widely been used for its antispasmodic effect; however, in terms of improving the ADR, a consistent increase has not been demonstrated. 17
Distal colonoscope attachments used as mucosal exposure devices can improve visualization of the colonic mucosa and highlight flat and subtle lesions. 18 The most widely used devices are a simple transparent cup and a cuff with one or two flexible wings. According to several studies, their use has a positive impact on adenoma detection, especially in the proximal colon.19,20
Dye chromoendoscopy has become essential for the identification of dysplasia and adenomas in patients with inflammatory bowel disease (IBD), 21 but the use of pancolonic chromoendoscopy also improves the ADR and particularly the detection of flat and small adenomas (<5mm) in patients without IBD. 22 Despite its efficacy, implementing the routine use of dye chromoendoscopy is not widely endorsed because it is time consuming and poses technical difficulties. A multimatrix methylene blue tablet has been used with promising results. 23
Electronic chromoendoscopy is a valid alternative to dye chromoendoscopy and may easily be applied with the press of a button, allowing better characterization of a lesion and differentiation of neoplastic lesions. However, results on the impact of virtual chromoendoscopy on the ADR are, at present, contradictory. As technology improves and new virtual chromoendoscopy systems are incorporated their potential impact on the improvement of ADR values seems promising. 24
References
- Rex DK, et al. Colorectal Cancer Screening: Recommendations for Physicians and Patients from the U.S. Multi-Society Task Force on Colorectal Cancer. Am J Gastroenterol 2017 Jul; 112: 1016–1030.
- Barret M, et al. Factors associated with adenoma detection rate and diagnosis of polyps and colorectal cancer during colonoscopy in France: results of a prospective, nationwide survey. PLoS One 2013; 8: e68947
- Rees CJ, et al. Expert opinions and scientific evidence for colonoscopy key performance indicators. Gut 2016; 65: 2045–2060.
- Jover R, et al. Modifiable endoscopic factors that influence the adenoma detection rate in colorectal cancer screening colonoscopies. Gastrointest Endosc 2013; 77: 381–389.
- Barclay RL, et al. Colonoscopic withdrawal times and adenoma detection during screening colonoscopy. N Engl J Med 2006; 355: 2533–2541.
- Lee TJ, et al. Longer mean colonoscopy withdrawal time is associated with increased adenoma detection: evidence from the Bowel Cancer Screening Programme in England. Endoscopy 2013; 45: 20–26.
- Butterly L, et al. Serrated and adenomatous polyp detection increases with longer withdrawal time: results from the New Hampshire Colonoscopy Registry. Am J Gastroenterol 2014; 109: 417–426.
- Jung Y, et al. Relationship between the endoscopic withdrawal time and adenoma/polyp detection rate in individual colonic segments: a KASID multicenter study. Gastrointest Endosc 2019; 89: 523–530.
- Nielsen AB, et al. Impact of feedback and monitoring on colonoscopy withdrawal times and polyp detection rates. BMJ Open Gastroenterol 2017; 4: e000142.
- Vavricka SR, et al. Monitoring colonoscopy withdrawal time significantly improves the adenoma detection rate and the performance of endoscopists. Endoscopy 2016; 48: 256–262.
- Rex DK. Polyp detection at colonoscopy: Endoscopist and technical factors. Best Pract Res Clin Gastroenterol 2017; 31: 425–433.
- Coe SG, et al. An endoscopic quality improvement program improves detection of colorectal adenomas. Am J Gastroenterol 2013; 108: 219–226.
- Lee SW, et al. Effect of dynamic position changes on adenoma detection during colonoscope withdrawal: a randomized controlled multicenter trial. Am J Gastroenterol 2016; 111: 63–69.
- Clark BT, et al. Yield of repeat forward-view examination of the right side of the colon in screening and surveillance colonoscopy. Gastrointest Endosc 2016; 84: 126–132.
- Rex DK. How I approach retroflexion and prevention of right-sided colon cancer following colonoscopy. Am J Gastroenterol 2016; 111: 9–11.
- Michopoulos S, et al. Su1671 Retroflexion in the ascending colon is a costless endoscopic maneuver increasing adenoma detection rate. Gastrointest Endosc 2019; 89 (Suppl): AB373.
- Rondonotti E, et al. The impact of hyoscine-N-butylbromide on adenoma detection during colonoscopy: meta-analysis of randomized, controlled studies. Gastrointest Endosc 2014; 80: 1103–1112.
- Gkolfakis P, et al. Colonoscopy attachments for the detection of precancerous lesions during colonoscopy: A review of the literature. World J Gastroenterol 2018; 24: 4243–4253.
- Nutalapati V, et al. Cap-assisted colonoscopy: a meta-analysis of high-quality randomized controlled trials. Endosc Int Open 2018; 6: E1214-E1223.
- Desai M, et al. Impact of cap-assisted colonoscopy on detection of proximal colon adenomas: systematic review and meta-analysis. Gastrointest Endosc 2017; 86: 274–281.e3.
- Pohl J, et al. Pancolonic chromoendoscopy with indigo carmine versus standard colonoscopy for detection of neoplastic lesions: a randomised two-centre trial. Gut 2011; 60: 485–490.
- Brown SR, et al. Chromoscopy versus conventional endoscopy for the detection of polyps in the colon and rectum. Cochrane Database Syst Rev 2016; 4: CD006439.
- Repici A, et al. Efficacy of per-oral methylene blue formulation for screening colonoscopy. Gastroenterology 2019; 156: 2198–2207.e1.
- Matsuda T, et al. Advances in image enhancement in colonoscopy for detection of adenomas. Nat Rev Gastroenterol Hepatol 2017; 14: 305–314.
-
About the authors
Spyros Michopoulos is Head of the Department of Gastroenterology at ‘Alexandra’ Hospital, Athens, Greece. He trained in medicine and completed his PhD thesis on “Erythromycin on Esophageal Motility” at the Medical School of Athens University. He trained in gastroenterology in Paris, France, where he worked in many university hospitals and undertook his clinical and research fellowship. He is a past President of the Hellenic Society of Gastroenterology (HSG), of the Hellenic Study Group for IBD and the Hellenic Study Group for Helicobacter pylori. He is President of the Educational Committee of HSG and belongs to the executive of the European Section and Board of Gastroenterology and Hepatology (ESBGH) of UEMS. His main research interests include gastrointestinal motility, endoscopy and H. pylori infection.
Georgios Axiaris is a gastroenterology trainee in the Department of Gastroenterology at Alexandra General Hospital, Athens, Greece. He was born in Serres and studied medicine at Aristotle University of Thessaloniki, Greece. His research interests include inflammatory bowel disease and endoscopy.





Please log in with your myUEG account to post comments.