Correct answer: d.
Discussion
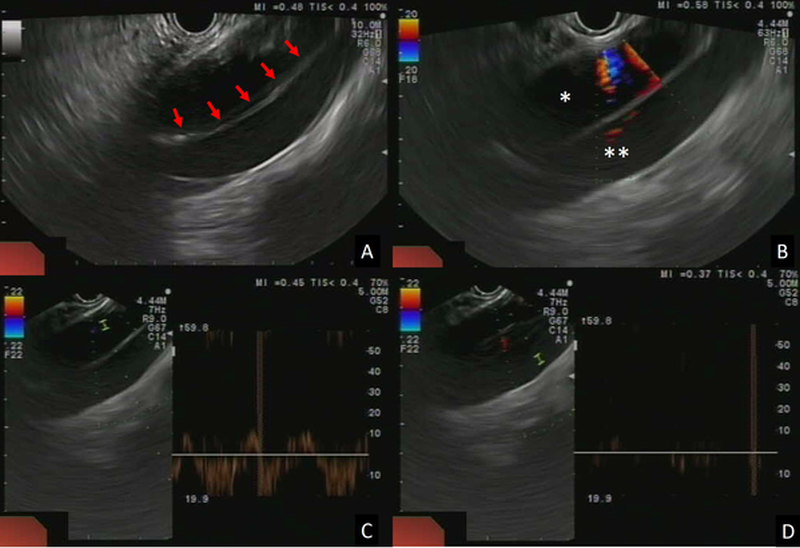
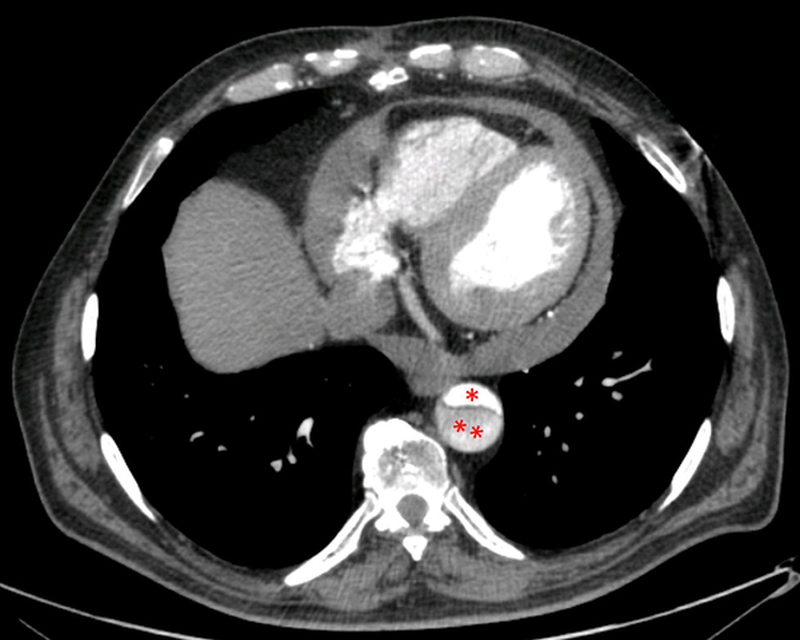
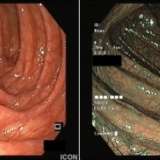
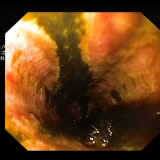
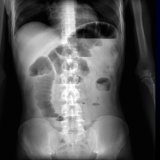
Following EUS examination (figure 1), the patient underwent a CT scan (figure 2) and was diagnosed with an aortic dissection confined to the descending thoracic aorta (Stanford type B). On the basis of the clinical characteristics, the patient was treated conservatively with medical therapy.1
Aortic dissection is a relatively common acute emergency, affecting 2–3 per 100,000 people per year. It usually presents with severe chest or abdominal pain, depending on which part of the aorta is affected. However, in a small number of patients, aortic dissection can have a subclinical course and remain unrecognized. In fact, in about 30% of patients, aortic dissection can be diagnosed in its chronic state.2 For Stanford type B chronic dissection, conservative treatment associated with strict monitoring of blood pressure is advisable. Actually, medical management has been demonstrated to be related to a lower mortality rate when compared with surgery (10% versus 30%).3
EUS has been shown to be useful not only for the study of gastrointestinal diseases, but also for mediastinal pathologies. Some case reports have been published showing the importance of EUS for the unintentional diagnoses of cardiovascular pathologies. Considering that EUS examination of mediastinal lymph nodes and cardiovascular system from the oesophagus takes about one minute and that cardiovascular diseases are potentially life-threatening, EUS-based mediastinal screening should be considered as a part of the standard EUS examination for gastrointestinal diseases.4


Please log in with your myUEG account to post comments.