Correct answer: C.
Discussion
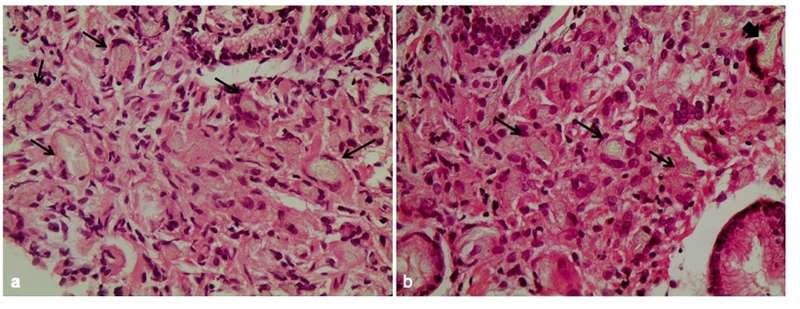
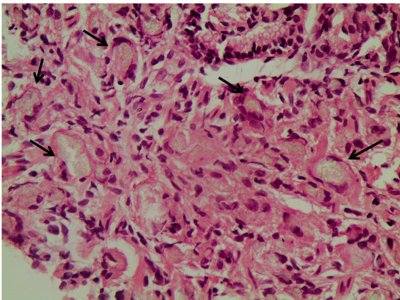
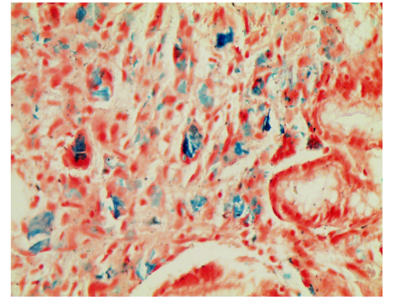
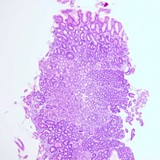
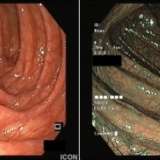
The histological findings shown in figure 1 indicate a proliferation of macrophages and the formation of granulomas in the antrum of the stomach (figure 2). When the presence of granulomas is confirmed in the stomach, a diagnosis of granulomatous gastritis (GG) is made. GG is a type of chronic gastritis and can either be secondary to an underlying condition (further subclassified as infectious or non-infectious) or an isolated finding with no specific identifiable cause (known as idiopathic GG). Idiopathic GG may account for up to 25% of all cases.1
GG is a rare finding, with an incidence of 0.08–0.35%; in the largest series to evaluate its epidemiology 56 cases were identified from a total of 15,947 tissue specimens.2
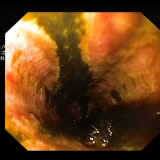
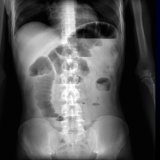
Patients with GG may exhibit epigastric pain, as in this case, but they may have no symptoms whatsoever. There have also been reports of patients with vomiting and weight loss due to gastric outlet obstruction. Bleeding as a manifestation of GG is exceedingly rare, but it has been seen, especially in patients for whom sarcoidosis is the underlying cause, and it may be massive and life threatening.3 There is also considerable variation in the endoscopic findings, which range from a macroscopically normal mucosa to the appearance of erythema, erosions and gastric rugae hypertrophy. In severe cases, there may be ulcers present or obstruction of the lumen due to mass effect similar to gastric malignancy.



Please log in with your myUEG account to post comments.