Correct answer: C.
Discussion
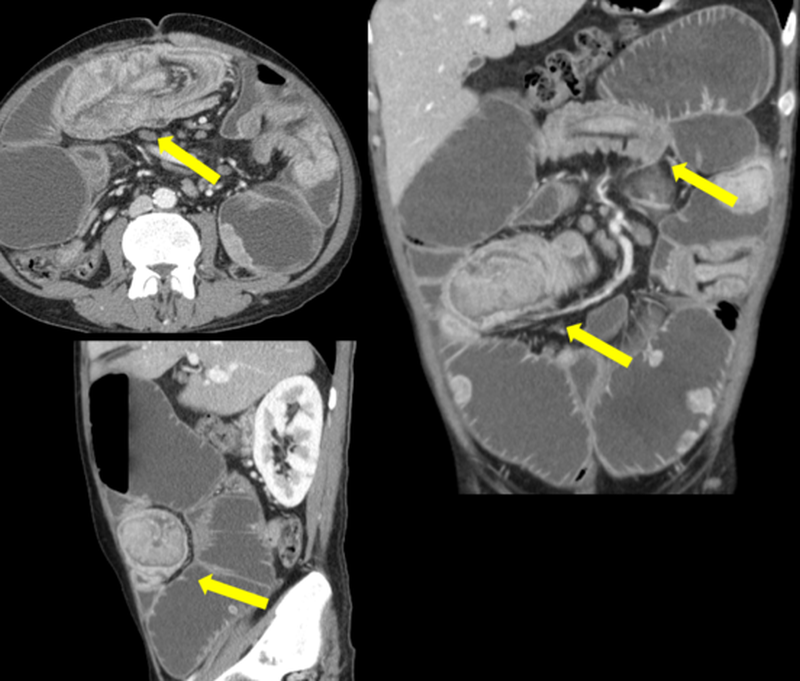
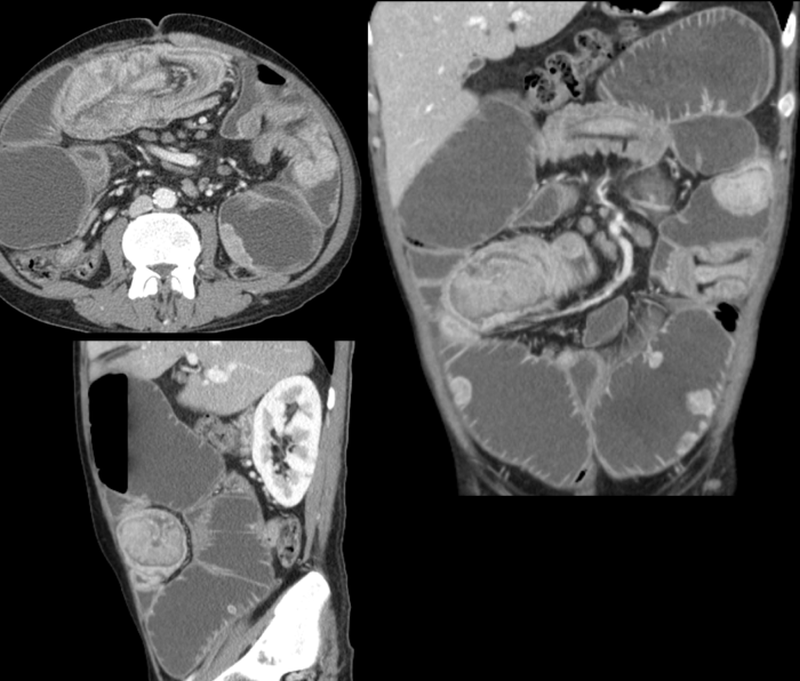
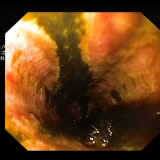
The yellow arrows on figure 3 indicate the presence of small bowel intussusceptions involving different segments of ileal loop in the case patient.
Intussusception is a serious condition in which part of the intestine slides into an adjacent part of the intestine. This ‘telescoping’ often blocks food or fluid from passing through the intestine. Intussusception also cuts off the blood supply to the part of the intestine that’s affected, which can lead to a tear in the bowel (perforation), infection and death of bowel tissue.1
Intussusception is the most frequent cause of bowel obstruction in paediatric patients;2however, it may occur in adults as the result of an underlying medical condition, such as a tumour, which may act as lead point, dragging part of the bowel into the neighbouring segment.3
There are several medical conditions/situations known to contribute to intussusception in adults:
- Congenital abnormalities (e.g. Meckel diverticulum, ectopic pancreas, duplication cyst)
- A polyp or tumour
- Scar-like tissue (adhesions) in the intestine
- Weight-loss surgery (gastric bypass) or other surgery on the gastrointestinal tract
- Gastrointestinal inflammation caused by disease (e.g. Crohn's disease)
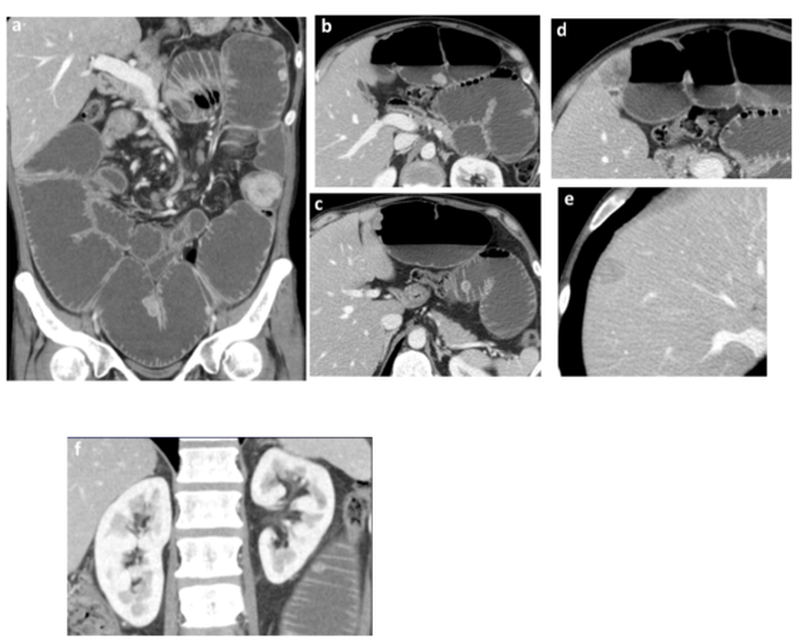
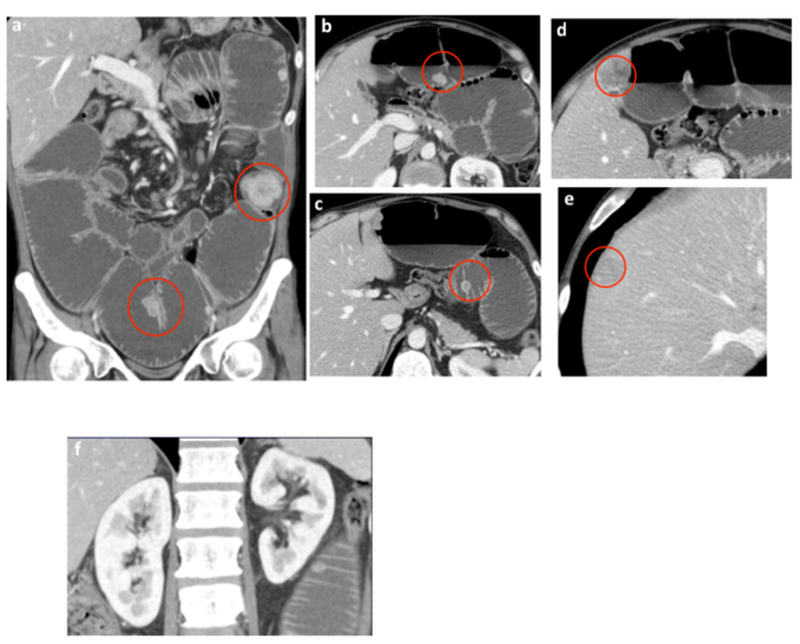
When intussusception occurs in adults, the most frequent symptom is abdominal pain that comes and goes. Nausea and vomiting may also occur. People sometimes have symptoms for weeks before seeking medical attention. A repeat CT scan was performed, and the findings are shown in figure 4.





Please log in with your myUEG account to post comments.