Correct answer: b.
Discussion
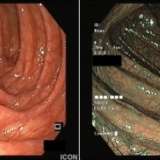
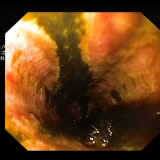
The duodenal mucosa is oedematous with engorged villi, but there is nothing to suggest either a pancreatic ampullary or duodenal carcinoma. The CT scan shows a diffusely enlarged (sausage-shaped) pancreas without dilatation of the pancreatic duct. This appearance is suggestive of autoimmune pancreatitis (AIP) and the serum IgG4 levels were found to be elevated.
AIP was first described in 1995 by Yoshida et al.1 The condition usually presents as a relapsing pancreatitis with recurrent obstructive jaundice and abdominal pain. Severe unremitting abdominal pain requiring opioids is unusual and should make you question your diagnosis. Less commonly, AIP presents subacutely with mild abdominal pain and elevated pancreatic enzyme levels and up to half of patients have diabetes. In the subacute phase, or after initial treatment, AIP can change into a clinical picture resembling chronic pancreatitis with pain, steatorrhoea and diabetes.
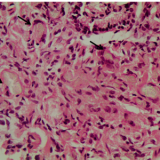
There are two distinct subtypes of AIP: type 1 AIP is characterized by a “lymphoplasmacytic sclerosing pancreatitis”2, whereas type 2 AIP is characterized by periductal infiltration with “granulocytic epithelial lesions”3.
Type 1 AIP is now recognised as a systemic IgG4-related disease that is associated with Sjögren syndrome, hilar lymphadenopathy, interstitial pneumonitis, sclerosing cholangitis, retroperitoneal fibrosis and tubulointestinal nephritis. By contrast, the only recognised association with type 2 AIP is inflammatory bowel disease.
AIP is probably under diagnosed and its true incidence unknown. However, AIP was diagnosed in 2–6% of patients who underwent pancreatic resection for suspected pancreatic cancer.4,5 In Japan the incidence of AIP has been estimated to be 0.82 per 100,000 population.6
On CT and MRI there are three recognized patterns. In diffuse disease there is a hypodense, sausage-like swelling of the pancreas with a sharp, smooth margin. Less commonly, there is focal disease with a relatively well-demarcated mass lesion within the pancreas (usually within the pancreatic head but any part may be involved); the lesion mimics pancreatic cancer, but with less upstream dilatation of the pancreatic duct than may normally be expected. The least common pattern is that of multifocal disease. Bile duct abnormalities are also common, such as a smooth narrowing of the intrapancreatic portion of the CBD, or irregularity of the intrahepatic and extrahepatic bile ducts (mimicking primary sclerosing cholangitis).
In type 1 AIP, the serum IgG4 levels are markedly raised (> 135 mg/dl) and ampullary biopsy samples may confirm that there is a lymphocytic infiltrate. In addition, an autoimmune profile may reveal the presence of anti-lactoferrin antibody (75%), anti-carbonic anhydrase II antibody (55%), antinuclear antibody (60%) or rheumatoid factor (20–30%).7 By contrast, IgG4 levels or autoantibodies are not found in patients with type 2 AIP and diagnosis hinges on a pancreatic core biopsy.
As up to 98% of AIP cases respond to therapy, a trial of steroids may be useful. Response is measured as a reduction in the size of the pancreatic swelling after 2–4 weeks of treatment. Naturally, if there is no improvement in either liver function test results or imaging, or the CA 19-9 level is rising, the diagnosis of AIP should be reconsidered. Conversely, if the disease is responding to treatment, the steroid dose is usually slowly reduced after week 4–6 as relapses are common, particularly in those who have the focal form of the disease.8 In the few patients who are intolerant of steroids or who are treatment resistant, rituximab (a monoclonal CD20 antibody) may induce remission. Patients with relapses may be considered for immunomodulators such as azathioprine, 6-mecrpatopurine, or mycophenolate; however, the relapse-free survival on an immunomodulator may not be very different to the outcomes of maintenance treatment with steroids alone.9


Please log in with your myUEG account to post comments.