Bjorn J. Rembacken is at Leeds Teaching Hospitals NHS Trust, Leeds, UK. He was born in Sweden and qualified from Leicester University in 1987. He undertook his postgraduate education in Leicester and in Leeds. His MD was dedicated to inflammatory bowel disease. Dr Rembacken was appointed Consultant Gastroenterologist, Honorary Lecturer at Leeds University and Endoscopy Training Lead in 2005.
Dealing with upper gastrointestinal (UGI) bleeding is fraught with pitfalls, not least because spotting those patients who are suffering significant bleeding can be difficult amongst the majority of referrals who are ill and hypotensive for other reasons. Despite diagnostic difficulties and the increasing age and comorbidities of our patients, the mortality rate from UGI bleeding has remained stable over the past 30 years.1–4 The variable mortality rates in published series can be explained by the inclusion of a proportion of healthier patients without a significant bleeding site. For this reason, the best way to assess emergency UGI bleeding outcomes is probably to exclude cases in which there is no significant finding, and only include patients with bleeding ulcers and varices into the calculated 30-day mortality rate. In Leeds we have examined the mortality rate in all patients with bleeding ulcers and varices over a 5-year period and found a 30-day mortality rate of 22%.5
In the absence of non-invasive means to identify patients with genuine bleeding, the benchmark for patients with emergency GI bleeding is to offer an emergency gastroscopy within 24 hours. In the UK, even this permissive benchmark is not always achieved. In a UK National audit,6 only 50% of patients underwent endoscopy within 24 hours of presentation, compared with 76% of patients in a Canadian audit.7
For patients with UGI bleeding, we know that early endoscopy is safe, reduces length of hospital stay and reduces the need for emergency surgery.8–12 However, we have no strong evidence that an early endoscopy saves lives.11–13 This may be as most series are small and largely composed of patients who do not have significant bleeding. Naturally, carrying out an emergency endoscopy in a patient who develops vomiting after commencing antibiotics for a bronchopneumonia is unlikely to make any difference to mortality.
Here, I draw on many years clinical experience to discuss the mistakes most frequently made when dealing with UGI bleeding.
© UEG 2016 Rembacken.
Cite this article as:
Rembacken BJ. Mistakes in upper gastrointestinal bleeding and how to avoid them. UEG Education 2016: 16: 15–19.
Correspondence to:
Conflicts of interest:
The author declare there are no conflicts of interest.
Published online:
May 25, 2016.
I recall the case of a young man who presented late one Friday evening following a haematemesis during my time as a junior doctor. He had a heart rate of 100 bpm and a blood pressure of only 95/60. Both his haemoglobin and urea were normal and there was no melaena. Nevertheless, I carried out an emergency endoscopy only to find a small Mallory–Weiss tear. In retrospect, I realised that the tachycardia was due to the patient’s anxiety and a blood pressure of 95/60 is normal in someone aged 18 years. My consultant declared that I should have applied the Blatchford Score to identify whether the patient was in need of emergency endoscopy.14
You should be familiar with the Blatchford system of scoring blood urea levels, haemoglobin levels (scored differently for men and women), systolic blood pressure, heart rate and the presence of melaena, syncope and underlying liver and heart disease. However, you should also be aware that critics of the initial study of the score were quick to point out that it contains circular reasoning. One of the main outcomes in the study was the need for blood transfusion. One of the most important predictors of a patient needing a blood transfusion was a haemoglobin level below 10 g/dL. That a low haemoglobin level predicts the need for a blood transfusion is hardly rocket science!
Not long after learning first hand the importance of risk profiling, a 30-year-old man presented late on a Saturday evening with a haematemesis, a heart rate of 110 bpm, a blood pressure of 110/80, no melaena and normal blood test results. His Blatchford score was only 1. Clearly then this was someone who could be discharged and an outpatient gastroscopy performed in the next few weeks. But this patient was sick, cold and sweaty, so I went ahead and performed an emergency endoscopy. This time I found an actively bleeding posterior duodenal ulcer! The bleeding had been so brisk that the ‘blood meal’ had not had time to travel down to the colon and present as melaena. Furthermore, the patient had no time to haemodilute and drop his haemoglobin levels. The following morning, my consultant agreed that it had been correct to carry out an emergency endoscopy and there was no talk of Blatchford scores.
These two cases taught me some valuable lessons. First, tachycardia is the best sign of ongoing bleeding. Second, if in doubt, recheck the blood pressure with the patient standing or at least sitting up. Third, the Blatchford score is unreliable, particularly when the bleeding is brisk.
Of course, at the bedside things can easily become confusing. For example, quite possibly your patient is on a beta blocker. CLARIFY is an international, prospective, observational, longitudinal registry of 33,438 patients with stable coronary artery disease.15 Although 75% of the patient cohort were beta blocked, the heart rate distribution was close to what would be expected in a non-beta-blocked population (figure 1). Indeed 44% had a resting heart rate above 70 bpm. Despite the fact that stable angina guidelines recommend a target heart rate of 55–60 bpm, the real-world experience is clearly different to the aspirational treatment targets.

Figure 1 | Heart rate distribution in stable coronary artery disease patients. From Steg PG, et al. Heart rate and use of beta-blockers in stable outpatients with coronary artery disease. PLoS ONE 2012; 7: e36284. doi:10.1371/journal.pone.0036284. Published under the Creative Commons Attribution (CC BY) licens
These findings are consistent with observations from the EuroHeart Survey on angina.16 As patients on beta blockers seem to have similar resting heart rates to those of non-beta-blocked patients, I now place less importance on the potential effects of beta blockers when evaluating patients.
The second case also taught me that decisions are always scrutinised by others with the benefit of hindsight. Nevertheless, assessing the Blatchford score helps provide a rationale for your decision. Indeed, if I had decided not to perform emergency endoscopy in the middle of the night, I could have justified my decision as the patient’s Blatchford score had been only 1 and the hospital policy was to not even admit patients with scores of 0 and 1.17
Most referrals to the emergency endoscopy services are from wards where elderly, frail patients have been admitted with some intercurrent illness and develop signs of bleeding. These patients may have a low Blatchford score, but if their Rockall score18 is high, they nevertheless require an emergency endoscopy. The reason for this is that the Rockall score is a measure of the risk of dying. It is sobering to realise that apart from the source of bleeding, the two main factors that predict death are the patient’s age and comorbidities.
That the old and ill are more likely to die than the young and fit is hardly surprising; however, by juxtaposing the Blatchford and the Rockall scores, you can develop a more nuanced argument. For example, “I decided not to endoscope this fit young man in the middle of the night although his Blatchford score was 4, because the pre-endoscopy Rockall score was 0, thus the risk of him dying of a bleeding ulcer was only 2%.” The calculation underpinning this statement is that, although the patient had a Blatchford score of 4, which is associated with a 40% risk of having a significant bleeding lesion, the post-endoscopy Rockall score could never be greater than 3, a score which is associated with a 2% risk of dying. As the mortality jumps to 10% if a patient with a Rockall score of 3 suffers a rebleed, I would organise an emergency endoscopy first on the morning list. Conversely, an out-of-hours emergency endoscopy may well be justified in an elderly, frail patient with a low Blatchford score but with a high pre-endoscopy Rockall score.
Currently, the treatment paradigm is to not perform endoscopy until a patient has been adequately resuscitated.19 The problem is that the patients with the most severe bleeding are in the greatest need of prompt endoscopy and the least likely to ever achieve haemodynamic stability. This issue is well recognised on the battlefield—patients receive blood and blood products continuously from the time of medical evacuation and into the operating theatre without delaying surgery until haemodynamic stability is achieved. This lesson from the battlefield may also be relevant to our elderly, comorbid patients who have a significant UGI bleed. A US study reported a significant survival benefit in patients randomly allocated to early resuscitation, including early correction of coagulopathy. The study was not designed to look at time to endoscopy, but observed a trend for earlier endoscopy in the intensive resuscitation group.20
Of course an emergency endoscopy in an unstable patient who has an active bleeding site is not a trivial undertaking. To protect the airway from aspiration, the patient should be intubated and monitored by an experienced anaesthetist. An experienced endoscopist who is fully trained in all treatment modalities for haemostasis should treat the bleeding site. The endoscopist should be supported by two experienced endoscopy assistants who are familiar with all the equipment and do not need prompting. At the same time another intensivist should be putting the hospital ‘massive transfusion protocol’ into action and liaise with laboratory personnel, the on-call vascular radiologist, GI surgeons and the intensive treatment unit.
Apart from potentially delaying a life-saving endoscopy, the doctrine of “resuscitate first and endoscope afterwards” has another unintended consequence—over transfusion.
A meta-analysis of studies of trauma, surgery and intensive care found that transfusion was associated with a greater risk of infection, multiorgan failure, acute respiratory distress syndrome and death than non-transfusion.21 The same has been shown in patients undergoing percutaneous cardiac interventions.22 An old UK study linked transfusion with increased risk of rebleeding 23 and the same trend was seen in the more recent 2007 UK audit of the use of blood in upper GI bleeding.4
Of course, an explanation may be ‘confounding by indication’, whereby patients with the most profuse bleeding are the most likely to receive blood and the most likely to die. However, there is circumstantial evidence that blood transfusions are not always beneficial. For example, although blood transfusion does increase oxygen delivery to tissues there is paradoxically no corresponding improvement in tissue oxygenation.24–27 There are several possible reasons for this: stored blood has low 2,3-diphosphoglycerate levels, stored cells are more rigid and probably more likely to get stuck in capillaries, and stored cells are low in vasodilatory nitric oxide. Stored blood is also pro-coagulant due to increased levels of plasminogen activator inhibitor. In fact, the longer blood has been in storage the less beneficial it appears to be. A study by Koch et al. reported a markedly increased mortality (2.8% vs. 1.7%) and more serious adverse events, such as renal failure, sepsis, multiorgan failure and the need for prolonged ventilatory support, in patients given older blood (>14 days) following cardiac surgery.28
Transfusion of colloids is falling out of favour because of concerns over the possible increased risk of death and acute kidney injury.29–32 The evidence is less than clear cut and in the recent CRISTAL trial of patients in intensive care with hypovolaemia, the use of colloids versus crystalloids was not associated with a significant difference in 28-day mortality.33 A Cochrane review of 2007, found no statistical difference in outcomes between crystalloids and a wide range of colloids.34
Most national GI bleeding guidelines still recommend “volume restoration prior to transfusion.” 35,36 I can see how resuscitating patients who have sepsis, burns or multiple trauma with fluids could make sense. However, in patients with hypovolaemia from blood loss, it is difficult to understand why the lost blood would not be best replaced with red blood cells, especially when most hospitals would be able to produce cross-matched blood within 30 minutes of receiving a request. The reason is that we have no evidence from randomized controlled trials, for or against early or large-volume intravenous fluid administration in the setting of uncontrolled haemorrhage.37
In an observational study of patients with acute bleeding and haemodynamic instability, patients who received intensive haemodynamic resuscitation had significantly fewer myocardial infarctions and lower mortality compared with those in the ‘observation’ group.20
Naturally, withholding blood transfusion when it is clearly indicated would also be a mistake. All UK hospitals have transfusion thresholds in place. The ESGE recommend a restrictive red blood cell transfusion strategy that aims for a target haemoglobin concentration between 7 g/dL and 9 g/dL.36 This advice was based on a single-centre Spanish trial of 921 patients presenting with UGI bleeding who were randomly allocated to a restrictive or liberal transfusion policy. Survival was 4% better in the restrictive transfusion group (95% versus 91%; confidence interval 0.33–0.92) who also had a reduced risk of rebleeding (10% versus 16 %; 95% CI 0.47–0.98).38 However, 21% of the trial population had variceal haemorrhage and 31% had cirrhosis. Furthermore, patients with ‘massive bleeding’ or the ‘usual comorbidities’ such as ischaemic heart disease, vascular disease or stroke were excluded from the study. Although no details were provided on the average age of the patients, the patient population does seem rather different from the norm.
The TRIGGER trial attempted to revisit the question of restrictive versus liberal transfusion in six UK centres without excluding elderly patients with significant comorbidities. Almost 1,000 patients were randomised, but surprisingly both the average haemoglobin level and average number of units transfused were not significantly different in the two groups and unsurprisingly there was no difference in outcomes.39 The reason for this unexpected finding was that clinicians proved very reluctant to transfuse patients, even when the patient had been randomly allocated to a liberal transfusion policy.
In any case, treatment targets may not be helpful in unstable patients with active bleeding. For this reason, the American Society of Anesthesiologists has rejected the use of rigid haemoglobin transfusion thresholds and recommends that the decision should be based on the clinical scenario.40 For example, a pilot trial of transfusion strategies in patients with ischaemic heart disease found a 15% excess mortality rate in patients only receiving blood when their haemoglobin dropped below 8 g/dL compared with those transfused once their haemoglobin dropped below 10 g/dL.41
For patients with UGI bleeding, NICE offers transfusion advice that can be summarised as follows:19
- Base decisions on blood transfusion on the full clinical picture, recognising that over transfusion may be as damaging as under transfusion.
- Transfuse patients with ‘massive bleeding’ with blood, platelets and clotting factors.
- Offer platelet transfusion to patients who are actively bleeding and have a platelet count of less than 50 x 109/L.
- Do not offer platelet transfusion to patients who are not actively bleeding and are haemodynamically stable.
The elephant in the room is the wording ‘active bleeding’, because how is it possible to determine if a patient is actively bleeding without an endoscopy? An early endoscopy allows early discharge of those without significant bleeding, prevents hazardous and unnecessary transfusion of blood products and focuses resources on those with significant bleeding.
Nowadays a large proportion of patients have a circulation that is only maintained with the aid of antithrombotic drugs. These drugs are potent. Many men on aspirin and clopidogrel decide to stop wet shaving, as the prolonged bleeding that results from a nick to the skin is unmanageable. The risk of GI bleeding is up to 12%42 in patients taking warfarin and even higher in patients treated with one of the newer anticoagulants.43
The elderly patient admitted with tachycardia, a grossly elevated prothrombin time and melaena is familiar throughout the western world. It is tempting to administer prothrombin complex concentrate with vitamin K and then recheck the prothrombin time and go ahead with the endoscopy once the prothrombin time has normalised. However, delaying the emergency endoscopy is a mistake. In fact, a British study found that there is no need to correct the coagulopathy in bleeding patients who have a prothrombin time of 2.5 or less.44 The study also found that even in patients with a prolonged prothrombin time, there was no need to wait for complete normalisation of the INR before carrying out the endoscopy. Admittedly, a UK audit of patients with non-variceal bleeding found that the risk of endoscopic treatment failure was greater with a prothrombin time >1.5.45 However, the study did not provide any details on whether the coagulopathy was due to anticoagulation or liver disease.
Reversing anticoagulation may not only be unnecessary but also hazardous. This is because reversing anticoagulation is associated with an increased risk of subsequent thrombotic events. In one study, nearly 17% of patients suffered a thrombotic event after reversal of their anticoagulation.46 An earlier study had put the figure at around 1%.47
The ESGE recommend that patients with cardiovascular disease should undergo prompt endoscopy for risk stratification.36 After endoscopy, those with a significant bleeding site should either have the aspirin stopped for 2 days, the second anti-platelet agent stopped for ‘a few days’ or warfarin stopped for 7 days. How long the new direct oral anticoagulants should be stopped for is less clear in the ESGE guideline.
There are no guidelines on what haemostatic interventions anticoagulated patients should receive. Personally, however, I would have a low threshold for providing ‘triple therapy’—injection of adrenaline, application of heat, and application of a haemostatic clip.
Another common scenario is that of an elderly patient with severe vascular disease who has been admitted with an acute coronary artery syndrome. A potent platelet inhibitor has been started, following which the patient develops haematemesis and melaena.
In this situation, does the risk of delaying the endoscopy outweigh the risk of triggering an arrhythmia? I personally believe that it does, but I am not aware of any data to support this. Should you now advise that the antiplatelet agent is stopped? A cardiologist is likely to tell you that stopping or reversing the antiplatelet therapy with a platelet transfusion will probably kill the patient.
A randomised study 48 found that patients taking aspirin for secondary prophylaxis were ten times more likely to die from cardiovascular, cerebrovascular or GI complications if the aspirin was stopped before the emergency endoscopy (1.3 % versus 12.9 %, 95 % CI 3.7 % – 19.5 %). Furthermore, the 30-day ulcer rebleeding rate was not significantly greater in the aspirin group.
The excess risk of death after stopping aspirin may not only be due to the hypercoagulable effect of GI bleeding. Stopping aspirin results in a rebound hypercoagulable state, as shown by an accumulation of the arachidonic acid metabolite 12-l-hydroxy-5,8,10-heptadecatrienoic acid,49,50 a rebound elevation in urinary excretion of thromboxane B2 and in 6-keto-PGF1-α.51
There are no randomised trials looking at the outcomes of emergency endoscopic intervention in patients with acute coronary syndromes. However, in my opinion the safest option would be to organise an early endoscopy, leaving the anti-thrombotic medication undisturbed. If it proves endoscopically impossible to stop the bleeding, early angiography is likely to be safer than attempting to reverse the anti-thrombotic therapy with platelet transfusions, haemodialysis or plasma transfusions.
Of course, emergency endoscopy must be carried out and everything done to try to stop the bleeding. But what if the bleeding cannot be stopped? Emergency surgery is linked with high mortality rates, averaging 29% in an audit by Jairath et al.45 Emergency surgery to undersew a bleeding ulcer after a myocardial infarction is likely to be even more hazardous. Luckily the mortality rate is far lower (10%) when patients are treated by arterial embolisation.45 For this reason, embolisation is now the secondary treatment of choice in all cases of failed endoscopic therapy.
There is agreement that bleeding peptic ulcers are best treated with endoscopic ‘dual therapy’—adrenaline injection, followed by the application of heat.52 But how to manage an ulcer with an overlying adherent clot? I used to be told not to touch it as the clot was there for a reason and was doing a job! However, the risk of rebleeding when the clot is not aggressively removed may be as high as 35% 53 or as low as 0–8%.54,55 One study reported a visible vessel below the clot in 70% of cases.54 In spite of this, the evidence for what to do is not clear cut. A meta-analysis of four trials did find a significant benefit from removing the clot (8.2% risk of rebleeding versus 24.7%; RR 0.30; CI 0.10–0.77).56 However, a subsequent meta-analysis found no significant benefit of endoscopic therapy for ulcers with adherent clots.57
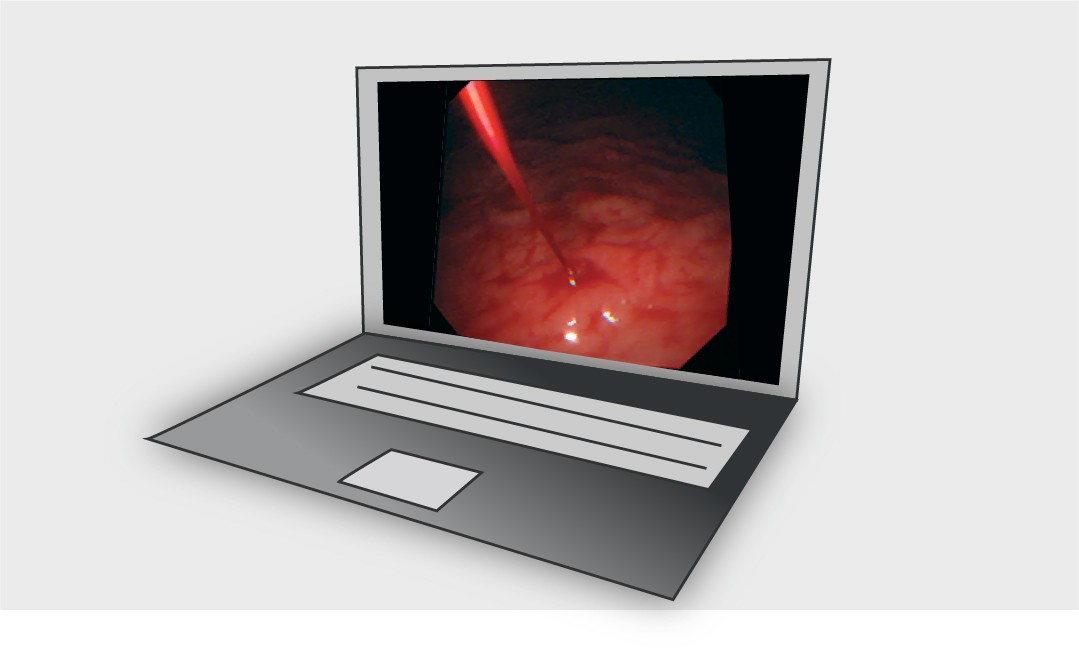
My own solution, anchored in experience rather than science, is to first observe the lesions for pulsation. The lesions with the highest risk of bleeding may have an aneurysmal dilatation of the underlying vessel. If I see pulsations, I apply a nearby clip and request transcatheter arterial embolisation. The clip forms a radio-opaque marker to guide the radiologist to the site of bleeding.
In the absence of any visible pulsations, I pre-inject below the clot with dilute adrenaline (1:100,000 solution) and apply suction with the tip of the endoscope. When bleeding is precipitated, I use haemospray that, in my hands at least, only seems effective when there is no overlying clot shielding the bleeding site from the powder. However, I must admit that I find it very difficult to avoid getting the tip of the haemospray catheter blocked by blood. Others have reported good results with the haemospray device, achieving initial haemostasis in up to 95% of cases.58
-
About the Author
-
Your upper gastrointestinal bleeding briefing
UEG Summer School
- ‘Session 4: Upper GI bleeding’ at UEG Summer School 2014.
UEG Week sessions
- ‘Video case session: Gastrointestinal bleeding’ at UEG Week 2015.
- ‘Digestive diseases in the elderly’ at UEG Week 2015.
- ‘Therapy update: Acute upper GI bleeding’ at UEG Week 2014.
- ‘Upper gastrointestinal bleeding (UGIB): Management and outcomes’ at UEG Week 2014.
- ‘Management of GI bleeding: A case based discussion’ at UEG Week 2013.
- ‘Management of Upper GI haemorrhage’ at UEG Week 2008.
Standards and Guidelines
- Gralnek IM, et al. Diagnosis and management of nonvariceal upper gastrointestinal hemorrhage: European Society of Gastrointestinal Endoscopy (ESGE) Guideline. Endoscopy 2015; 47: 1–46.
- SIGN. Guideline 105. Management of acute upper and lower gastrointestinal bleeding. September 2008.
- National Institute for Health and Clinical Excellence. Clinical Guideline 141: Acute upper gastrointestinal bleeding: Management. 2012.
- Barkun AN, et al. International consensus recommendations on the management of patients with nonvariceal upper gastrointestinal bleeding. Ann Intern Med 2010; 152: 101–113.
Please log in with your myUEG account to post comments.