Correct answer: a.
Discussion
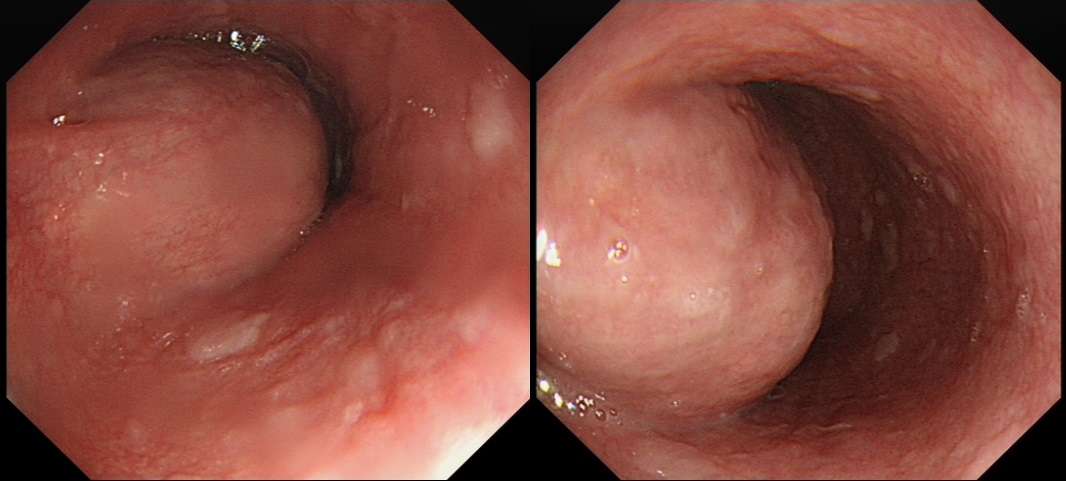
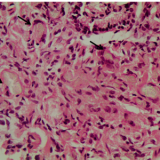
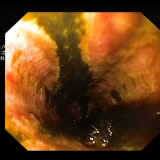
The endoscopic images show a submucosal swelling in the distal oesophagus. Of course, the most likely diagnosis would be a leiomyoma. However, both the ultrasound and the CT show that the lesion is cystic. Although a pericardial cyst would be a possibility, the only cystic lesion on the shortlist is the duplication cyst!
Gastrointestinal duplication cysts are formed during early embryonic development via abnormal budding or development of the primitive gut.1 These cysts are rare entities, with only two being found in one paediatric autopsy study of 4,000 patients.2 Because of their rarity, information on location, patient characteristics, complications and treatment outcomes is derived from case reports and small case series. They can occur at any point along the gastrointestinal tract and multiple lesions can be found throughout.3 Oesophageal duplication cysts are found as one of two separate entities, being either a distinct mass or in continuity with the oesophagus with duplication of the muscularis mucosa.3 Presentation typically occurs in early childhood with symptoms related to their anatomical location, namely dysphagia, nausea, vomiting, respiratory distress, retrosternal pain or more rarely cardiac dysfunction and arrhythmia.3 If the cyst contains gastric-type mucosa then haemorrhagic transformation or peptic ulceration leading to possible perforation can occur. Other known complications include infection and there have been rare case reports of malignant transformation.4
Duplication cysts can be seen on routine upper gastrointestinal endoscopy as submucosal lesions causing a bulge in the oesophageal lumen or a diverticulum. They are better characterized by cross-sectional imaging with CT or MRI. Endoscopic ultrasound can then be useful to examine the lesions in more detail and differentiate them from solid masses. The diagnosis is best made via radiological features alone as fine-needle aspiration can precipitate infection.
Typically, the management of duplication cysts is now performed surgically by video-assisted thorascopic surgery (VATS) with good outcomes and prognosis, but care must be taken as the cysts can share the blood supply of the normal bowel.3 There is a case report of a successful endoscopic procedure to ‘de-roof’ the cyst and leave the cystic cavity exposed to the oesophageal lumen.5 If asymptomatic, it is reasonable to leave the cysts in situ after discussion with the patient about the potential complications. Post-operatively there is no indication for surveillance in asymptomatic patients.
With increased use of endoscopy and cross-sectional imaging we may expect more reports of incidental oesophageal duplication cysts. For symptomatic patients with, for example, pain, dysphagia, compression of a bronchus or a complication such as inflammation, rupture or infection of the cyst, surgical intervention via VATS is less invasive than open surgery. Endoscopic procedures are possible, but there is limited evidence for their use in this setting. For asymptomatic patients, conservative management may be appropriate, leaving intervention until symptoms occur. Surveillance for incidental lesions is probably not warranted. A quick Medline review only revealed a single report, published more than 30 years ago, of a squamous cell carcinoma arising within an oesophageal duplication cyst.



Please log in with your myUEG account to post comments.