Correct answer: D.
Discussion
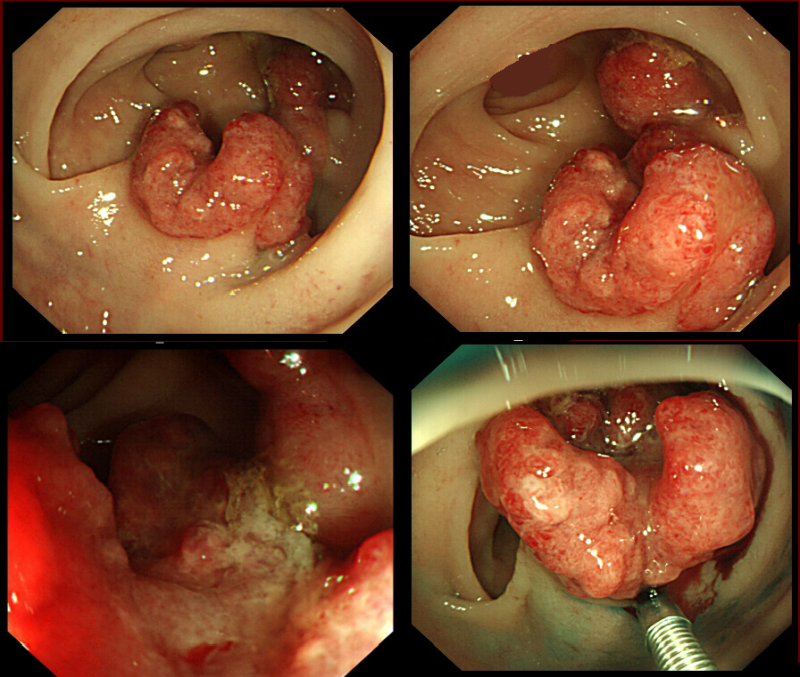
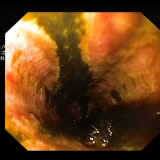
Clearly, this polyp is likely to be malignant. However, for some reason I decided to attempt a ‘test lift’ injection of colloid/adrenaline/indigo carmine dye into the submucosa. To my surprise the polyp lifted without any sign of tethering (bottom-right image) and I was able to remove it as a single fragment. The polyp turned out to be a tubular adenoma with a small spot of cancer in the centre.
Haggitt staging is the classic histological staging of the extent of invasion of cancers arising within pedunculated polyps.1
- Level 0 = Carcinoma in situ or intramucosal carcinoma (Haggitt level 0 lesions are not recognised in the UK because British histopathologists want to see malignant cells invading below the muscularis mucosa before they label a polyp as malignant).
- Level 1 = Carcinoma invading through the muscularis mucosa into the submucosa, but limited to the head of the polyp.
- Level 2 = Carcinoma invading the level of the neck of the adenoma.
- Level 3 = Carcinoma invading any part of the stalk.
- Level 4 = Carcinoma invading into the submucosa of the bowel wall below the stalk of the polyp, but above the muscularis propria.
Histopathologists may, however, be reluctant to apply the Haggitt classification because they can often have difficulty distinguishing the important boundaries between the head and neck and the neck and stalk of the polyp. These boundaries are arbitrary and subject to interobserver variability. Furthermore, if the stalk has been cut just below the head of the polyp, it will be impossible to diagnose a Haggitt level 4 lesion.
Naturally, all cancers staged as Haggitt level 4 are referred for further therapy. However, in Haggitt’s original publication, lymph-node metastases were also found in 6 out of 24 patients with Haggitt level 3 lesions.1
For flat lesions, cancers are staged using the Kikuchi classification.2 The risk of lymph-node metastasis for Kikuchi levels sm1, sm2 and sm3 is 2%, 8% and 23%, respectively.3 Unfortunately, it is difficult to use the Kikuchi system as there is normally no muscularis propria within the endoscopic resection fragment (unless you have cut too deep and perforated the colon of course).
In this particular case, the endoscopist would have noted that there is no discernable crypt pattern in the centre of the lesion. The endoscopist may well have made an endoscopic diagnosis of a ‘massively invasive cancer’ (i.e. cancer invading deeper than 1mm below the muscularis mucosa) and not have attempted resection. However, the detection of a suspicious crypt pattern (severely distorted crypt pattern or no pattern at all) has less relevance in pedunculated polyps, in which lesions can still be endoscopically resectable even if the tip of the lesion harbours a cancer.
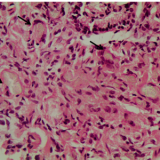
This polyp is also a good example of the practical difficulties our histopathologists may encounter when attempting to apply the Haggitt and the Kikuchi staging systems. Is this lesion pedunculated or sessile? In this case it is neither, and neither the Haggitt nor the Kikuchi staging system applies! Because of such difficulties, Japanese histopathologists instead rely on simply measuring the depth of invasion beyond the muscularis mucosa.4 Lesions invading less than 0.5 mm (i.e. <500 µm), are regarded as Kikuchi level 1 (sm 1 invasion), 500–1,000 µm as level 2 invasion and >1,000 µm as level 3 invasion.
In this case, the depth of invasion was <500 µm and the deep margin was clear by several mm. In addition, no adverse features were found within the polyp (i.e. it was a well-differentiated cancer without any lymphovascular invasion). For these reasons, we decided not to offer the patient any further treatment beyond polypectomy.

Please log in with your myUEG account to post comments.