Correct answer: d.
Discussion
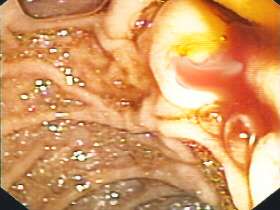
If you look more carefully at the photograph you can see blood trailing away below the bile. This patient has haemobilia.
Classic haemobilia was first described in 1654 by Francis Glisson.1 However, the first documented case report is attributed to Antoine Portal in 1777!2 The classic clinical presentation of bleeding into the biliary tract is of ‘Quincke’s triad’: gastrointestinal haemorrhage, biliary colic and jaundice. The typical biliary colic has been attributed to clots forming in the biliary tree, but it has also been suggested that substances in bile prevent the development of clots. An alternative possibility is that the pain is due to distension of the biliary tree by free-flowing blood.
Naturally, haemobilia is usually associated with percutaneous liver procedures such as percutaneous cholangiography, cholecystectomy or abdominal trauma. Less commonly haemobilia arises when a splanchnic vessel pseudoaneurysm has developed a communication with the intrahepatic or extrahepatic biliary system. The most common offending vessels include the cystic artery or the hepatic artery. Fistulas between the hepatic artery and the portal vein are less common. Finally, a pseudoaneurysm of the inferior gastroduodenal artery communicating with the pancreatic duct is decidedly rare!
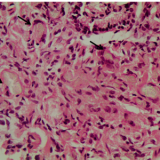
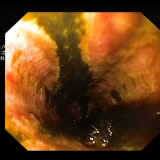
The preferred investigation for haemobilia is angiography because it allows therapeutic intervention. The case patient underwent selective arteriography, which confirmed a pseudoaneurysm of the inferior pancreaticoduodenal artery and chronic pancreatitis. The aneurysm was successfully embolised with polyvinyl alcohol particles (figure 2). Embolisation is now the treatment of choice rather than surgical repair.

Please log in with your myUEG account to post comments.