Dr Christen Rune Stensvold is a Senior Scientist and Public Health Microbiologist with specialty in parasitology. He has a Bachelor degree in Medical Sciences, an MSc in Parasitology, and a PhD in Health Sciences. He has been based at Statens Serum Institut, Copenhagen, since 2004. Since 2006, he has authored/co-authored more than 80 articles in international, peer-reviewed scientific journals. In 2013, he was awarded the Fritz Kauffmann Prize for his contribution to clinical microbiology in Denmark. For many years, he has been pursuing the role of common intestinal micro-eukaryotes in human health and disease. Follow Rune on Twitter @Eukaryotes.

According to the ICD-11 Beta draft, “functional dyspepsia is a disorder defined as the presence of dyspepsia symptoms thought to originate from the gastroduodenal region, in the absence of any organic, systemic, or metabolic disease that is likely to explain the symptoms such as epigastric pain, epigastric burning, postprandial fullness, and early satiation.”1
Functional dyspepsia may affect up to at least 20% of the population.2 Faced with patients who have dyspeptic symptoms, physicians are constantly challenged by the need to discriminate functional dyspepsia from organic disease of the stomach or duodenum.
Using gastrointestinal endoscopy, it has been demonstrated that less than 10% of patients with dyspepsia have a peptic ulcer, less than 1% have gastroesophageal cancer, and more than 70% have functional dyspepsia.3 Hence, organic disease is only rarely identified in patients with dyspepsia, which is one of the reasons why performing endoscopy in all patients with these symptoms is not practical. Even when limiting endoscopy to those patients presenting with ‘alarm symptoms’ (i.e. age >55 years with new-onset dyspepsia, gastrointestinal bleeding, dysphagia/odynophagia, persistent vomiting, unintentional weight loss, a family history of gastric/oesophageal cancer, a palpable abdominal/epigastric mass and/or evidence of iron-deficiency anaemia), the predictive value of such symptoms is low, since only a few of the tested cases will be diagnosed with gastroesophageal cancer or another life-threatening disease.4
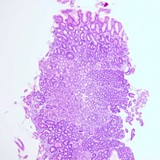
Helicobacter pylori is quite possibly the most successful human pathogen, infecting an estimated 50% of the global population.5 It is a common and curable cause of peptic ulcers, but is also linked to the development of gastric cancer. About 5% of functional dyspepsia may be attributable to H. pylori infection.6
In populations in which the prevalence of H. pylori infection is at least 10% (which is almost everywhere), it is recommended that noninvasive screening of patients (typically younger, i.e. <45 years of age) with dyspeptic symptoms using either the urea breath test or a stool antigen test should be performed (the so-called test-and-treat strategy).7,8 However, the proportion of infected patients who experience resolution of their dyspepsia symptoms upon H. pylori eradication in prospective trials is low (number needed to treat >10). Moreover, there are no criteria available to predict whether or not infected patients who have dyspeptic symptoms will respond clinically to eradication therapy.9 Nevertheless, the current view is that for infected patients who have symptoms of dyspepsia, H. pylori eradication therapy is better than placebo, and so H. pylori eradication is the preferred option in patients presenting with dyspepsia in the absence of alarm symptoms.9
Only patients presenting with dyspepsia in the presence of H. pylori and who remain symptomatic upon successful H. pylori eradication should be diagnosed with functional dyspepsia.9 Importantly, patient evaluation with regard to symptom relief should be carried out at least 6–12 months following H. pylori eradication to avoid any effect of placebo and because of the fact that it would “…take some time…” to recover from gastritis-induced atrophy.10
Unwanted effects of eradication therapy must also be considered. First, the development of multiple-drug resistance due to widespread use of antibiotics, including imperfect compliance with eradication therapy, has made treatment of H. pylori difficult in some communities.11 Second, observational studies have raised concerns that H. pylori eradication can lead to gastro-oesophageal reflux disease (GORD).12 Prospective trials have not confirmed this in the short to mid term (indeed, H. pylori infection appears to ‘protect’ patients from reflux and its complications13,14); however, recovery of gastric acid secretion over the long term could exacerbate symptoms in patients who have a weak reflux barrier (e.g. hiatus hernia).13 Finally, proponents of the so-called hygiene hypothesis are concerned that eradication of H. pylori infection could increase the risk of autoimmune disorders (e.g, eczema or multiple sclerosis) in vulnerable individuals.15,16
Meanwhile, in several Western countries, the prevalence of H. pylori infections appears to be in decline and, indeed, this effect may be linked to the increase in GORD in these populations.17,18 Based on this evidence, Talley and Ford question the relevance of the test-and-treat strategy in such countries and recommend that in settings where the local prevalence of H. pylori is <10%, treatment should rely on the clinical presentation. These authors suggest that if postprandial distress syndrome with excessive fullness, bloating, nausea and pain after meals is present, then a trial of a prokinetic agent should be considered (the choice of prokinetic should consider local availability, drug interactions and the risk of long-term complications); alternatively, and in other cases, empirical acid suppression therapy should be given for 4–8 weeks.10
To read more about the challenges related to the diagnosis and treatment of patients with dyspeptic symptoms in clinical practice, I encourage you to take a look at “Mistakes in dyspepsia and how to avoid them”.19
References
- ICD-11 Beta draft. http://apps.who.int/classifications/icd11/browse/f/en [accessed February 2016].
- Tack J, Talley NJ, Camilleri M, et al. Functional gastroduodenal disorders. Gastroenterology 2010; 131: 1466–1479. http://www.sciencedirect.com/science/article/pii/S0016508506005087
- Ford AC, Marwaha A, Lim A, et al. What is the prevalence of clinically significant endoscopic findings in subjects with dyspepsia? Systematic review and meta-analysis. Clin Gastroenterol Hepatol 2010; 8: 830–837. http://www.sciencedirect.com/science/article/pii/S154235651000563X
- Vakil N, Moayyedi P, Fennerty, et al. Limited value of alarm features in the diagnosis of upper gastrointestinal malignancy: systematic review and meta-analysis. Gastroenterology 2006; 131: 390–401. http://www.sciencedirect.com/science/article/pii/S0016508506008407
- Malfertheiner P, Megraud F, O’Morain CA, et al. Management of Helicobacter pylori infection—the Maastricht IV/Florence consensus report. Gut 2012; 61: 646–664. http://gut.bmj.com/content/61/5/646.long
- Moayyedi P, Forman D, Braunholtz D, et al. The proportion of upper gastrointestinal symptoms in the community associated with Helicobacter pylori, lifestyle factors, and nonsteroidal anti-inflammatory drugs. Am J Gastroenterol 2000; 95: 1448–1455. http://www.nature.com/ajg/journal/v95/n6/abs/ajg2000375a.html
- Talley NJ, Vakil NB, and Moayyedi P. American Gastroenterological Association technical review on the evaluation of dyspepsia. Gastroenterology 2005; 129: 1756–1780. http://www.sciencedirect.com/science/article/pii/S0016508505018184
- Talley NJ and Ford AC. Functional Dyspepsia. N Engl J Med 2015; 373: 1853–1863. http://www.nature.com/nrgastro/journal/v12/n10/full/nrgastro.2015.158.html
- Sugano K, Tack J, Kuipers EJ, et al. Kyoto global consensus report on Helicobacter pylori gastritis. Gut 2015; 64: 1353–1367. http://gut.bmj.com/content/64/9/1353.long
- Suzuki H and Mori H. Helicobacter pylori gastritis—a novel distinct disease entity. Nat Rev Gastroenterol Hepatol 2015; 12: 556–557. http://www.nature.com/nrgastro/journal/v12/n10/full/nrgastro.2015.158.html
- Thung I, et al. Review article: the global emergence of Helicobacter pylori antibiotic resistance. Aliment Pharmacol Ther 2016; 43: 514–533. http://onlinelibrary.wiley.com/doi/10.1111/apt.13497/abstract
- Labenz J, et al. Curing Helicobacter pylori infection in patients with duodenal ulcer may provoke reflux esophagitis. Gastroenterology 1997; 112: 1442–1447. http://www.ncbi.nlm.nih.gov/pubmed/?term=9136820
- Schwizer W, et al. The effect of Helicobacter pylori infection and eradication in patients with gastroesophageal reflux disease: a parallel-group, double-blind, placebo-controlled multicenter study. United European Gastroenterology Journal 2013; 1: 226–235. http://ueg.sagepub.com/content/1/4/226.abstract
- Kandulski A and Malfertheiner P. Helicobacter pylori and gastroesophageal reflux disease. Curr Opin Gastroenterol 2014; 30: 402–407.http://journals.lww.com/co-gastroenterology/pages/articleviewer.aspx?year=2014&issue=07000&article=00012&type=abstract
- Luther J, et al. (2010). Association between Helicobacter pylori infection and inflammatory bowel disease: a meta-analysis and systematic review of the literature. Inflamm Bowel Dis 2010; 16: 1077–1084. http://journals.lww.com/ibdjournal/pages/articleviewer.aspx?year=2010&issue=06000&article=00026&type=abstract
- Wang Q, et al. The association between asthma and Helicobacter pylori: a meta-analysis. Helicobacter 2013; 18: 41–53. http://onlinelibrary.wiley.com/doi/10.1111/hel.12012/abstract
- Delaney BC, Qume M, Moayyedi P, et al. Helicobacter pylori test and treat versus proton pump inhibitor in initial management of dyspepsia in primary care: multicentre randomised controlled trial (MRC-CUBE trial). BMJ 2008; 336: 651–654. http://www.bmj.com/content/336/7645/651.long
- Agréus L, Talley NJ and Jones M. Value of the “Test & Treat” strategy for uninvestigated dyspepsia at low prevalence rates of Helicobacter pylori in the population. Helicobacter Epub ahead of print 8 September 2015; DOI: 10.1111/hel.12267. http://onlinelibrary.wiley.com/doi/10.1111/hel.12267/abstract
- Fox, M. Mistakes in dyspepsia and how to avoid them. UEG Education 2016; 16: 4–6. https://www.ueg.eu/education/latest-news/article/article/mistakes-in-dyspepsia-and-how-to-avoid-them/
-
About the Author






Please log in with your myUEG account to post comments.