Correct answer: e.
Discussion
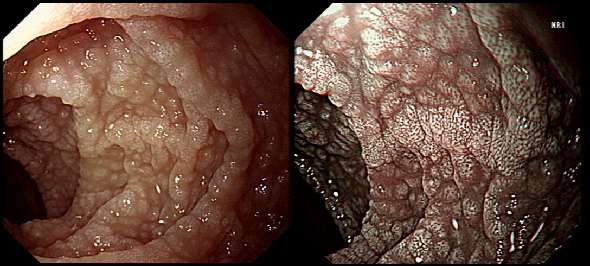
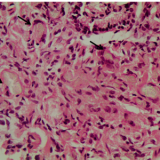
Initially, the patient appeared to have classic coeliac disease, with diarrhoea and weight loss together with a positive serology. The endoscopy was crucial as the duodenal biopsies identified the presence of a thick band-like deposit of collagen just below the duodenal epithelium. On the basis of this finding, collagenous sprue was diagnosed.
Collagenous sprue was first described in 1947,1 but it was not until 1970 that Weinstein et al. introduced it as a diagnostic term to the medical nomenclature.2 Collagenous sprue is more frequent in females and in individuals who have other autoimmune diseases.3 It is now recognised that collagenous sprue shares similar clinical features with coeliac disease, such as chronic diarrhoea, anaemia and weight loss. In addition, the endoscopic and histological features of both diseases are similar, with an atrophic and scalloped duodenal mucosa. However, the histological hallmark of collagenous sprue is the presence of a thick subepithelial collagen band. Such collagen bands may also be found in collagenous gastritis and collagenous colitis.4
It has been proposed that collagenous sprue may be a heterogenous condition of collagenous gastroenteritides, including conditions such as collagenous colitis and coeliac disease.5,6 Unlike coeliac disease, in collagenous sprue, the typical histological changes may also be found in the stomach and colon.7 Furthermore, greater numbers of IgG4 plasma cells have been reported in the duodenal mucosa of patients with collagenous sprue when compared with the numbers in patients with coeliac disease, duodenitis or normal duodenal mucosa.8
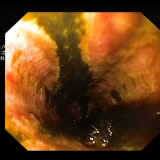
As in this case, patients with collagenous colitis usually also have positive coeliac serology. For this reason, some believe that the collagen band is simply a marker of particularly severe coeliac disease, which may also be associated with ulceration, perforation and T-cell or B-cell lymphoma.9
An interesting report of paraneoplastic collagenous colitis was reported by Freeman et.al.10 In that case a patient with collagen deposits in both the small and large intestine was also found to have a coincidental colon cancer. After surgery, both the malabsorption and the histopathological changes completely resolved! For this reason, a search for underlying malignant disease should be considered.
The response to a GFD is usually disappointing, and for this reason the outlook used to be grave for patients with collagenous sprue. However, remission of the condition has been reported with courses of corticosteroids11 or immunosuppressive agents such as infliximab.12

Please log in with your myUEG account to post comments.